Do you ever feel like your vagina is pressing into your vulva? Or that you have shooting pains in your bits like knitting needles? Is it uncomfortable to walk at times? You are not alone!
Itching, burning and sore vulvas, vaginal dryness, painful sex, feeling like you have thrush or a urine infection can all be signs that you have vulvo-vaginal atrophy (VVA).
VVA is widely reported to affect 70% of menopausal women but as only around 7% get treatment, that figure could actually be far higher.
Lisa told me she had no idea what was happening to her when her symptoms first started a few months ago at 49. She thought she was suffering a prolapse or scarily worse. None of her friends she spoke to knew either. Catherine said the pain was so intense at times it was as if knitting needles were being poked into her vagina. At its worse, Jacqui could not sit down or walk, the pain was so excruciating. All these women were subsequently diagnosed with VVA but not without a fight to get their symptoms taking seriously.
VVA doesn’t just affect women of a certain age. Freya first noticed symptoms 8 weeks after having her baby. Within a week she had become more aware of pain in her vagina and inner labia (the lips of the vulva) while walking, and progressively symptoms became even more painful with a feeling that the vagina was putting pressure on the vulva.
After birthing a 9lb baby 6 months earlier, my GP told me that the discomfort I was having was due to having been stitched too tight (yikes) and a new diagnosis of lichen sclerosis so I was referred to a gynaecologist. By the time I got to see the gynaecologist several months later, I’d stop breastfeeding and my tightness had resolved. At no point was I told by my GP that my reduced oestrogen enabling me to breastfeed was causing my vagina to be tight.
My blog on the wonders of our cervical fluid touched on how oestrogen can affect how much cervical fluid we might have. Oestrogen levels can drop at any time, but typically happens during times of stress, breastfeeding and perimenopause as well as after menopause.
Menopause (when a woman has not had a period for over 12 months) is usually preceded by some years where periods are irregular – the ‘perimenopause’ (unless menopause is medically or surgically induced) and includes the hot flushes we all know about, as well as joint and muscular pain, mood changes, brain fog, a lower sexual desire and urogenital problems. Every woman is different.
This is all caused by a decrease in oestrogen which affects every tissue in our body including those in our bladders and vaginas. With less oestrogen, our vaginas shorten and narrow and the lining becomes thinner and less elastic. Cervical fluid is reduced and vaginal PH changes. All symptoms of VVA, part of ‘genitourinary syndrome’ (GSM).
Vaginal dryness is probably the most talked about symptom of VVA. However, dryness implies something that can be sorted out with a bit of moisturiser in the right place. It does not do justice to the wide ranging symptoms of VVA and the sheer pain and discomfort women feel. As it is the cells that are affected the vagina itself may still feel moist even though there are symptoms of VA.
Whilst it is a natural part of the ageing process, treatments are available which can really help symptoms.
In the UK on the NHS, options include:
Other things you can try to help VVA include:
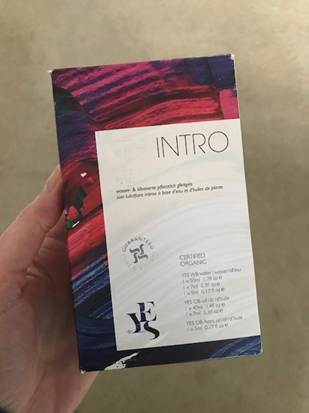
There are many products available over the counter but they are not all created equal. The vagina has its own microbiome (like your gut) and can be more sensitive to ingredients in products when oestrogen deficient. Some contain ingredients that can irritate and burn so a more natural product like YES or vegan and organic Into the Wylde may suit some women better. They can be used on their own or in combination with systemic or topical hormone replacement therapy. It can take trial and error to find one that suits you but it is worth persisting. Some have hyaluronic acid which helps plump up and brings significant temporary relief such as Canesintima.
There are some suggestions that increasing blood flow to the vagina with regular sexual activity may help. However, all the women I spoke to said that even a finger was too big when their VVA was at its worst, due to pain and tightness. This suggestion apportions blame to a woman who may already be feeling frustrated with their bodies and guilty. Which is not warranted and unjust.
Dr Catherine Pestano (an Early Career researcher at the University of Winchester and who is currently running an open menopause research group) feels that most women don’t understand what is happening to them and so cannot describe it to doctors. Doctors are also likely to be unaware of what is happening to the women they see in front of them. I apologise to any doctors who do understand VVA but the reality is that ALL the women I spoke to had to see several doctors before they were taken seriously and many women resorted to seeing a private doctor before they received adequate treatment. I even heard of one woman being asked why she wanted treatment for VVA when she wasn’t having sex!
VVA has an extensive effect on a woman’s’ quality of life, yet is not widely discussed, is underreported and undertreated. That needs to change. If you think you have VVA talk to your doctor. Ensure you get treatment and if that treatment doesn’t work persist with seeking medical advice. Dr Pestano said that there are other conditions that can co-occur or seem like VVA or are often part and parcel of the changes during menopause. For example, bacterial vaginosis or Lichen Sclerosus which can cause intense itching. And so, addressing this can bring some elements of relief with products such as bioflor and canesflor. You can also be referred to a menopause specialist. Do not suffer in silence and assume this is just part of getting older.
I’m sure this won’t be my only exploration of this issue. I’d love to hear your own experience and what has worked or not worked for you. Thank you to the women who spoke to me candidly about their symptoms.
Becca x
Menopause Did you Know?
References:
Resources and Women raising awareness of Menopause and VA
Menopause NICE Guidelines: https://www.nice.org.uk/guidance/ng23/resources/menopause-diagnosis-and-management-pdf-1837330217413
The British Menopause Society
Vaginal Atrophy Self Help Facebook Group
Davinia McCall and her Documentary – Sex, Myths and the Menopause available on All4
Meg Matthews and her new book – ‘The New Hot, taking on the menopause with attitude and style (2020), Vermilion, UK.
Turning Back the Clock on Your Vagina – Lauren Streicher, (2021), USA
Me and My Menopausal Vagina: Living with Vaginal Atrophy – Jane Lewis, (2018), PALS, UK
Naomi Potter and Lisa Snowden on Instagram
Davinia Taylor on Instagram
Menopause and Employment Law – https://henpicked.net/category/menopause-hub/menopause-and-work/